The Centre for Aging + Brain Health Innovation (CABHI) recently selected 40 projects to participate in the Spark program, which supports the development of grassroots innovations by frontline healthcare workers and researchers to solve real-world care challenges.
Through Spark, CABHI will invest over $1.9 million in support of these 40 projects, which range from a dementia empathy training toolkit for care partners of people living with dementia to a first-of-its-kind low-cost, personalized, remotely-managed virtual reality intervention program that can improve visual perception in older adults. While unique, each project shares a common goal: improving the quality of life for older adults, people living with dementia, and caregivers.
Read about the 40 projects below:
Assessing & Supporting Caregivers in Residential Care: The Canadian Caregiver Adjustment Needs Tool (C-CANT)
Project Lead: Adriana Shnall
Organization: Baycrest (Ontario)
Theme: Caregiver Support
Supporting a loved one with dementia is an important but often strenuous endeavour. Informal/unpaid caregivers in the community frequently experience burnout accompanied by high caregiving burden. This project aims to enhance caregiver support during this transitory period by adapting and piloting a caregiver assessment tool. Results will be used to directly inform care plans and to improve the relevance and quality of support services offered to caregivers.
This assessment will be initially piloted with family caregivers of residents at the Memory Terrace unit at Baycrest. This innovation will allow Baycrest to address a significant worldwide gap in understanding how to best support families of people that are institutionalized, as well as contribute to emerging research on when and how to properly assess residents’ families’ needs.
Development, validation, and implementation of a tool to predict life expectancy among frail community-dwelling individuals with dementia
Project Lead: Michael Bonares
Organization: Bruyère Research Institute (Ontario)
Theme: Care Coordination & Navigation
Individuals living with dementia and their caregivers face challenging decisions about healthcare, institutionalization, or financial planning. A clinical prediction tool has the promise to provide personalized and accurate estimations of life expectancy in individuals living with dementia. This tool – a user-friendly, web-based calculator – uses self-reported sociodemographic, clinical, cognitive, functional, and nutritional information entered by patients, their caregivers, and/or their healthcare providers to output an estimated life expectancy.
The tool could become a foundational component of decision-making among individuals living with dementia, their caregivers, their healthcare providers, inextricable from the medical history, physical examination, laboratory, and imaging investigations that currently inform decision-making.
Feasibility of high-accuracy indoor positioning and smart home technologies for assessing and monitoring older adults
Project Lead: Antonio Miguel-Cruz
Organization: University of Alberta, Glenrose Rehabilitation Hospital (Alberta)
Theme: Aging in Place
Frailty screening today is conducted on a non-routine basis in primary care or clinical settings; as a result, “hidden health vulnerabilities” cannot be identified early enough and, therefore, frailty prevention is not possible.
This solution is a non-camera-based tracking technology with sensors and smart biomechanical devices embedded in older adults’ daily activities at home (thus preserving autonomy and privacy. It generates meaningful frailty data for older adults, caregivers, and the healthcare system. In addition, it is based on the concept of Zero Effort Technologies, so frail older adults do not need to develop new skills to use this monitoring system to manage frailty.
Help for Helpers: A Caregiver Navigation Guide available on YouTube
Project Lead: Kendelle LaBella
Organization: WoodGreen Community Services (Ontario)
Theme: Care Coordination & Navigation
The Caregiver Navigation Guide is a series of approximately twenty informational videos on topics identified by East Toronto Health Partner’s Caregiver Advisory Group, spanning the over-arching navigation topics of: Introduction to Navigation, Navigating a Hospital stay, Legal Considerations, PSW Care at Home, Community Programs, and “Right Place of Care” – Options for living arrangements beyond care at home. The topics are broken down into smaller sections, with several short (under 5 minute) videos covering each of the six areas of information.
This guide walks caregivers through foundational knowledge with the aim of building their toolbox of information and resources, to better equip them in their caregiving journey. Through community promotion, the Caregiver Navigation Guide will help transform adverse outcomes into positive ones for caregivers and their care recipients, by increasing access to resources that are codesigned, free to access, meaningful, relatable, and culturally sensitive/appropriate.
Improving Chronic Disease Management Through Brain Health – Intersectional approach for older adults and caregivers with Health Inequities
Project Lead: Heather Beaton
Organization: Nova Scotia Health (Nova Scotia)
Theme: Cognitive & Mental Health
Primary Health Care supports individuals to stay well and manage chronic conditions through dedicated services, resources, and programing. Our evaluation data suggests we are often not reaching the communities who need this support the most. To address this ever-growing concern, we will develop and refine wellness and chronic disease management supports for populations experiencing health inequities.
This project will use an intersectional best practice approach to develop and refine supports for older adults and their caregivers living with chronic conditions. The resulting program will:
- Be developed with community
- Leverage self-management support approaches
- Include wellness and chronic disease management strategies
- Focus on modifiable risk factors to delay cognitive decline
- Integrate research, best practice and experience
By working directly with our communities that have health inequities to co-design, deliver and evaluate we can ensure that the programs are embedded into the community infrastructure and promote a social network which is a key social determinant of health.
Creating Care and Connections: A Journey in Dementia Education
Project Lead: Ken Donohue
Organization: Haven Hill Retirement Centre (British Columbia)
Theme: Caregiver Support
The “Creating Care and Connections” initiative, led by SafeCare BC in collaboration with the Alzheimer’s Society of British Columbia, will help to improve the delivery of person-centred care through the development and delivery of online education and training. These short, online modules will enhance the ability of point-of-care staff to communicate with and provide person-centred care to people living with dementia. The modules will be designed to be easily accessible (from home or work), self-paced and quick to complete.
The “Creating Care and Connections” initiative will address the priority theme of caregiver support by increasing access to person-centred care education focused on older adults living with dementia. This training will give frontline workers concrete strategies and approaches to create meaningful connections with those that they care for every day. Importantly, this training will increase the confidence of frontline workers to manage some of the most common behaviours associated with dementia, including de-escalating those behaviours that have the potential to result in injury.
Virtual Reality as a non-pharmacological leisure intervention to reduce responsive behaviors in a LTC’s Transitional Behavioral Support Unit
Project Lead: Mara Swartz
Organization: Baycrest (Ontario)
Theme: Cognitive & Mental Health
A Transitional Behavioral Support Unit is where individuals with dementia who have noted responsive behaviors that are unmanageable in their current environment are admitted to from across the spectrum of care (other long-term care homes, hospitals, community). Virtual reality has been used in the TBSU at Baycrest’s long-term care home, the Jewish Home for the Aged, since 2021 for leisure and recreational purposes with positive observations.
Building on the know-how and lessons learned to date cultivated by the TBSU’s recreation therapist and identifying a gap in the literature as an opportunity to both contribute to the body of knowledge in applying this technology to this population and disseminate to other behavioral support units, this study will collect data in a more structured way to validate the hypothesis that virtual reality can be an effective leisure and non-pharmacological intervention to help reduce and stabilize behaviors. As a result, virtual reality can be used as a tool to improve the quality of life for behavioral clients.
Virtual Caregiver Support Program
Project Lead: Danielle Turpin
Organization: Home Care Workers Co-operative Inc. (Ontario)
Theme: Caregiver Support
The Virtual Caregiver Support Program (VSCP) will develop an online network of mental and physical experts to assist healthcare providers in dealing with the difficulties inherent in their jobs. The VCSP will develop online materials distributed through an interactive website and social media network to caregivers across Canada.
The hub of the VCSP will be an interactive website composed of informational and educational videos on a wide range of health topics targeted to healthcare providers. The VSCP website will promote the development of a caregiver network through open group chats, story sharing and interviews (video and print).
The Caregiver’s Network addresses the caregiver’s support priority providing a comprehensive approach to supportive care for caregivers including mental, physical and spiritual supports. The Caregiver’s Network will provide both formal and informal supports for caregivers providing care for older adults living with dementia.
The Mobile Social
Project Lead: Chelsey Roberts
Organization: Alzheimer Society Southwest Partners (Ontario)
Theme: Aging in Place
The “Mobile Social” is a group therapeutic recreation program for individuals living with dementia. The program meets a dual need, offering three hours of meaningful engagement to clients on a weekly basis while giving their care partners vital respite time. The program and staff will travel throughout our region to smaller centres where community-based, inclusive, and dementia-friendly recreation programs have not been available to people in the early to mid-stages of the disease.
The Mobile Social is designed with a dual purpose to help older adults age in place by offering a supportive and engaging therapeutic recreation program while at the same time ensuring care partners get a weekly break to look after their own needs.
A care partner’s role is complicated and generates significant stress related to direct care, navigating the healthcare system, emotional support and much more. As dementia progresses, most care partners experience a decrease in quality of life as they have less and less time to care for themselves.
Optimizing technology-based innovations to support aging at home and caregivers using a Portable Co-design Lab
Project Lead: Charlene Chu
Organization: Lawrence S. Bloomberg Faculty of Nursing, University of Toronto (Ontario)
Theme: Aging in Place
This project, a collaborative effort between rehabilitation, home care, and long-term care (LTC), will optimize three technology-based interventions targeting key problems that contribute to older adults’ healthy aging across the care continuum:
- smart-textile bedsheet for older adults in LTC;
- smart-home system for older adults with and without dementia and their caregivers;
- a mobile health symptom management application for older adults and their caregivers.
A Portal Co-design Lab will be used to increase accessibility and engage traditionally excluded groups by bringing the innovation to them ensuring diversity and representation in co-creators. At its conclusion, this project will result in the optimization of 3 technology-based innovations to support aging-at-home for a more diverse group of older adults and caregivers in different settings, as well as develop a Portal Co-design Lab that will contribute to improved knowledge of best practices for co-design of technology innovations with older adults.
 The Finger Foods Project: Preventing Malnutrition and Promoting Independence in Hospitalized Older Adults Living with Dementia
The Finger Foods Project: Preventing Malnutrition and Promoting Independence in Hospitalized Older Adults Living with Dementia
Project Lead: Maria Ghobrial
Organization: Trillium Health Partners (Ontario)
Theme: Cognitive & Mental Health
The Seniors Care Unit (SCU) is an 18-bed acute care unit focused on the care of older adults with complex health issues at Trillium Health Partners (THP). Through our proposal, our SCU Team aims to increase caloric consumption, improve food satisfaction, and improve ability to self-feed among patients living with dementia through the development and pilot of a Finger Foods menu option.
This project is one of the first to trial a Finger Foods menu option among people living with dementia in an acute-care setting within Canada. If successful, the Finger Foods menu option has the potential to be expanded across our entire hospital system to all patients living with dementia. Most importantly, the Finger Foods menu offers people living with dementia and in hospital accessibility to food as a basic human right, ensures human dignity, and leverages the power of food in recovery.
 Integrating Virtual Reality Reminiscence Therapy into Alzheimer Society of Durham’s Region Behavioural Support Lending Program
Integrating Virtual Reality Reminiscence Therapy into Alzheimer Society of Durham’s Region Behavioural Support Lending Program
Project Lead: Winnie Sun
Organization: Ontario Tech University (Ontario)
Theme: Cognitive & Mental Health
Our study is a project collaboration from the Advancement for Dementia Care Centre (a partnership between Ontario Tech University and Ontario Shores Centre for Mental Health Sciences), and point-of-care workers at Alzheimer’s Society of Durham Region (ASDR). This project aims to integrate the use of Virtual Reality (VR) Reminiscence Therapy into ASDR’s Behavioural Support Lending Program. Reminiscence therapy is a multi-sensory treatment that uses a combination of sight, touch, taste, smell, and sound to help people with dementia remember events, people, and places from their past lives.
The objective of our project is to evaluate the potential use of VR Reminiscence Therapy, to support people with dementia through ASDR’s Behavioral Lending Program, which provides Montessori-based approaches to managing responsive behaviours of people with dementia at home. Our goal is to develop micro-credential educational training, resources, and support to equip the care partners related to the use of VR reminiscence tool in complementary to the traditional responsive behaviour mitigation interventions.
A Multimodal Toolkit for Assessing Frailty at Home
Project Lead: Charlene Chu
Organization: KITE-Toronto Rehabilitation Institute, University Health Network (Ontario)
Theme: Aging in Place
“Multimodal Toolkit for Assessing Frailty at Home” is a passive at-home monitoring home sensor system to collect multimodal sensor data that can be used to detect the onset of frailty and conduct frailty risk stratification. This portable toolkit uses cutting-edge sensors connected to a cloud-based framework and uses advanced machine learning algorithms to assess the onset of frailty. The toolkit consists of 5 types of non-invasive off-the-shelf sensors (smart watch, motion sensor, smart scale, sleep mat, and dynamometer) and assesses frailty by measuring mobility, sedentary behaviour, weight, stair climbing time, and life space. The sensors automatically collect and send data over to a secured cloud and are accessible through a bespoke mobile application to the OAs and caregivers. The impact of early recognition of frailty will support caregivers and healthcare professionals by alerting them about at-risk older adults, enabling timely and appropriate assessments and care plans that support aging at home.
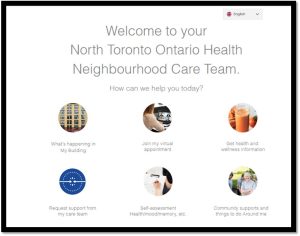 Tech Spot Virtual Health Booths – Concept Development and Analysis
Tech Spot Virtual Health Booths – Concept Development and Analysis
Project Lead: Einat Danieli
Organization: Baycrest (Ontario) in collaboration with the Toronto Seniors Housing Corporation Integrated Service Model
Theme: Care Coordination & Navigation
Our Tech Spot project will create and develop Virtual Health Booths in centralized locations within four high-priority North Toronto Seniors Housing buildings. The tech booth interface will enable low to moderate-income tenants living in supportive housing to access user-friendly, digital interfaces via Wifi-enabled tablets or their own devices. These free tablets and their senior-friendly interface will afford users the ability to navigate health services via the touch of a button and provide access to their local care team, health-related self-assessment tools, and other needed resources. Virtual Health Booths are a much-needed resource that can help address the tech challenges that seniors face in accessing care, such as poor connectivity, inability to afford devices or internet subscriptions, and language barriers.
Cognitive Stimulation Therapy for People Living with Mild-Moderate Dementia on Northern Vancouver Island
Project Lead: Alison Ritchie
Organization: Vancouver Island Health Authority (VIHA) (British Columbia)
Theme: Cognitive & Mental Health
This project delivers an evidence-based, non-pharmacologic intervention for mild-moderate dementia to northern Vancouver Island. No cognitive therapy treatment options are otherwise available for people with early dementia despite pressing current and future need; the local population is older than the Vancouver Island average and the 75+ age group is projected to grow rapidly in future years. Our Comox Valley Geriatric Specialty Services team is filling this gap through the introduction of cognitive stimulation therapy (CST), a well-evidenced, standardized treatment program delivered in a small group setting with people living with dementia. Research shows that CST can improve cognitive functioning, mental health, and quality of life; it also provides respite and support for family caregivers.
The objective of this project is to optimize the cognitive and mental health of people living with dementia (PLWD) through the delivery of CST, the only evidence-based cognitive intervention for mild-moderate dementia, which is part of the standard of care in the UK (NICE, 2018).
Development of evidence-based guidelines and an evaluation framework for dementia-specific bathroom design
Project Lead: Andrea Iaboni
Organization: Toronto Rehabilitation Institute (Ontario)
Theme: Caregiver Support
Bathing is a private and highly personal ritual that promotes relaxation or a sense of rejuvenation. It is also one of the first activities of daily living with which people living with dementia need assistance. Unfortunately, in long-term care (LTC), bathing can be stressful for people with dementia. The experience can generate fear or a sense of violation, and the process is often undignified and in conflict with the need for privacy.
Using person-centred care as a guiding principle, and with a strong project steering group including expertise in design, dementia care, and lived experience, this project will synthesize the current evidence and in a co-design process, develop guidelines and an evaluation framework for bathroom design in dementia care residential settings. These guidelines will be used to design and evaluate a bathroom renovation on the Specialized Dementia Unit at Toronto Rehab (TRI-SDU) and will be disseminated to designers and organizations involved in LTC home design to set the standard for person-centred bathroom design.
Validation of heart rate variability measurement using wearable technology to remotely monitor cognitive and mental health in older adults
Project Lead: Linda Mah
Organization: Baycrest (Ontario)
Theme: Cognitive & Mental Health
A major barrier to identifying older adults who are at risk for developing cognitive decline or dementia is the lack of cost-effective and accessible screening tools. This project will determine whether assessment of heart rate variability (HRV), defined as the variation in the time interval between consecutive heartbeats, can serve as a marker of risk for cognitive decline and dementia. HRV is a well-established indicator of cardiac and emotional health, with higher HRV associated with a healthier heart and greater emotional well-being.
This project will identify a novel indicator of risk for cognitive decline or dementia based on assessment of heart rate variability (HRV), which can be passively measured using existing wearable technology (Apple Watch). HRV can serve as a sentinel and as an objective measure to complement subjective report of cognitive decline. The proposed project will improve our ability to identify which older adults are at greatest risk for developing dementia and cognitive impairment so that interventions such as lifestyle change or clinical trials, can be introduced early.
Re:Garde Program: Training and maintaining visual perception in older adults to promote quality of life and prolong independence
Project Lead: Michael Reber
Organization: OpenLab, UHN (Ontario)
Theme: Aging in Place
Visual impairments can comprise the health and wellbeing of older adults. Maintaining good vision in older adults could help maintain good health, independence, and possibly reduce the risk of age-related cognitive declines such as dementia.
Re:Garde is the first low-cost, personalized, remotely-managed program that can improve visual perception. This Virtual Reality (VR) intervention, previously validated in clinical trials at the DJK Eye Institute at Toronto Western Hospital, will provide seniors the opportunity to train and improve their vision by using the Re:Garde program in a community setting.
West Kootenay Nav-CARE Scale-Up
Project Lead: Erin Thompson
Organization: Greater Trail Hospice Society (British Columbia)
Theme: Aging in Place
Nav-CARE is a compassionate community-based program that aims to improve the quality of life of adults living with chronic illness, social isolation, or increased frailty. Nav-CARE provides volunteers with a specially designed training centered on the quality of life concerns experienced by adults with declining health. Volunteers are then matched 1:1 with clients to assist with the client and family priorities. Volunteers have the luxury of time to engage, listen, support decision-making, and assist clients with practical things that help to meet their needs.
The program is evidence-based and built on research led by Dr. Barbara Pesut, PhD Canada Research Chair in Health, Ethics and Diversity at UBC, and Dr. Wendy Duggleby, Research Chair in Aging and Quality of Life, of the University of Alberta.
Developing a blueprint for a Community Paramedic-driven food insecurity screening and referral intervention for older adults with dementia
Project Lead: Krystal Kehoe MacLeod
Organization: Bruyère Research Institute (Ontario)
Theme: Aging in Place
This project will develop and disseminate a blueprint for integrating the community paramedic role in other primary care settings to facilitate the spread of community paramedics as a tool to address food insecurity in older adults living with dementia.
The approach includes:
- Screening older adults living with dementia on the community paramedic patient roster for food insecurity using a standardized assessment tool.
- Educating and/or referring food insecure older adults living with dementia to food resources to alleviate food insecurity and improve dietary quality.
- Evaluating the community paramedic role in the family health team context with an emphasis on work related to clinical food insecurity screening and referral.
Check your hearing, change your life!
Project Lead: Sylvia Ciechanowski
Organization: Baycrest (Ontario)
Theme: Cognitive & Mental Health
Hearing is important for social connectedness and mental and cognitive health. Hearing loss exacerbates social isolation through its adverse effects on communication and has been identified by the Lancet Commission as the leading potentially modifiable risk factor for dementia.
This innovation is an online hearing screening tool that Baycrest Hearing Services have customized and linked to hearing care via a phone consultation with an audiologist. The plan for this project is to take the next step in establishing hearing screening as a routine component of health care for older adults. Starting with Baycrest, this project aims to begin by focusing on programs for those most at risk for dementia, namely the Memory Clinic and Possibilities Program, by integrating hearing screening into their clinical pathways. Further, the team plans to include hearing screening into intake assessment protocols at the Terraces of Baycrest and Baycrest@Home. This funding would also enable them to investigate the extent to which screening leads to uptake of hearing help and how this benefits individuals and their caregivers, addressing an important risk factor for dementia.
A Day in the Life‚ Dementia Empathy Training through Role-Play
Project Lead: Justine Henry
Organization: The Centre for Innovation and Research in Aging (New Brunswick)
Theme: Care Coordination & Navigation
Dementia: Understanding the Journey is a dementia empathy training toolkit for care partners. The toolkit trains and empowers them in person-centred approaches when caring for people living with dementia. The training contains a handbook with different scenarios and props, including scripts, that small groups of staff members can use to act out commonly occurring situations among people living with dementia (i.e., an unmet need) as well as an online training and resource community to maintain momentum and deepen product implementation.
In 2019, Canada released a new Dementia Strategy confirming the need to prioritize the quality of life for people living with dementia. This toolkit aims to address these priorities by providing a better life for Canadians living with dementia.
SHPCA Road Show 2023
Project Lead: Mary-Anne Parker
Organization: Saskatchewan Hospice Palliative Care Association (Saskatchewan)
Theme: Care Coordination & Navigation
The Saskatchewan Hospice Palliative Care Association’s road show aims to address concerns surrounding rural end of life care delivery by delivering a series of rurally-based education sessions/workshops and informal meeting opportunities during which participants will explore supports already in place in their communities, identify ways in which knowledge can be shared throughout the region, and the development of a provincial-wide knowledge network that acknowledges the spectrum and progression of care requirements as we age. The over-arching goal of this initiative is to support our community elders in aging where they wish and in a manner which respects their wishes and values.
Enriching home-based vital signs for virtual care in older adults
Project Lead: Jonathan Afilalo
Organization: Jewish General Hospital (Quebec)
Theme: Aging in Place
Virtual care has upended the way people seek medical care due to its convenience and accessibility, allowing healthcare providers to meet patients where they are. In addition to playing a pivotal role in pandemics or remote regions with underserved populations, virtual care has become a preferred approach for outpatient care of older adults.
HealthStat seamlessly incorporates a series of medical devices into virtual care. By integrating with existing telemedicine providers, the team is designing a platform to automate all the steps to provide patients with one week of home monitoring of blood pressure, heart status, body composition, activity, and more, as part of a virtual visit. By replacing the 5-minute in-office spot check of vitals with 7 days of data, we can better manage chronic diseases, shift visits out of the hospital, reduce preventable ER visits, and empower aging in place.
Homeward: a tablet app program designed to enhance post-surgery recovery and wellness in elderly patients after emergency surgery
Project Lead: Eric Hyun
Organization: Saint-Boniface Hospital (Manitoba)
Theme: Aging in Place
Elderly patients generally require more care and longer hospital stay after undergoing emergency surgery. The goal of the program is for enhanced in-patient stay and safe/efficient discharge of elderly patients from the hospital to back home. The app assesses the cognitive/physical capabilities of the patients as well as assesses their home support needs for advanced discharge planning. Patients and caregivers are given tablets linked through the homeward app to stay connected during the hospital stay. The app also addresses common questions or concerns faced by patients after surgery and gives an option for communication between the health care professionals and patient/care-giver. The apps will feature preventative tools to avoid post-operative confusion or delirium. Lastly, the app will assist in discharge planning, especially by providing information about existing social programs and government agencies to aid the transition from hospital to home.

Passive Aware for At-Home Informal Dementia Care
Project Lead: Justine Henry
Organization: Centre for Innovation and Research in Aging (CIRA) (New Brunswick)
Theme: Aging in Place
Passive Aware uses passive ambient home monitoring technology to help older adults age in place successfully and reduce the stress and burden placed on their informal caregivers. The Passive Aware system uses non-intrusive sensors that keep track of the movement of items within the older adult’s home that are important to their daily functioning. Informal caregivers can then receive a notification or check in on the movement of the sensors through a personalized account. In the pilot stage of our project using this technology in the community, we have received feedback indicating that this solution may help reduce feelings of caregiver stress and worry, and also empower informal caregivers to allocate their care resources in a specific, personalized, and more efficient-manner.
Caring for dementia patients at home: creating a risk-communication tool to inform caregivers of the timing and risk factors of distress
Project Lead: Wenshan Li
Organization: Bruyère Research Institute (Ontario)
Theme: Caregiver Support
We aim to create a risk communication tool for caregivers of individuals with dementia living in the community. This tool will identify caregivers at high risk of distress, identify modifiable risk factors to address, and inform caregivers of services and support that can reduce distress. We have the following objectives:
- Objective 1: Describe the characteristics (e.g., age, sex, whether resided in retirement homes) of individuals with dementia in Ontario who have remained in the community and compare them to the characteristics of those who transitioned into LTC.
- Objective 2: Describe the proportion of caregivers who are distressed over their years of caregiving, highlighting in particularly whether retirement homes and home care services impact distress levels.
- Objective 3: Identify factors that increase or reduce caregivers’ likelihood of becoming distressed.
- Objective 4: Develop a tool to communicate the risk of caregiver distress and burden according to care-recipients’ characteristics, health, and receipt of services.
Mitigating health risks for long-term care residents using early detection of changes based on real-time location data
Project Lead: Kathleen Norman
Organization: Shannex (Nova Scotia)
Theme: Cognitive & Mental Health
Shannex is implementing nurse call bell systems that include real-time location in our long-term care and retirement living residences. These systems provide a mobile call bell device that is worn by the resident. The system reports on the location of residents within the building in real-time allowing staff to find those who need assistance. The system provides powerful data collection which translates into large amounts of real-time location data on all residents.
This data provides a previously untapped opportunity to monitor resident wellbeing and to mitigate adverse events. Our team will use this data to generate algorithms to understand typical behaviour patterns for residents and to then identify behavioural patterns fall outside their individual normal range. These changes in behavioural patterns will provide a window of opportunity to address changes in a resident’s cognitive function. By flagging an intervention window, clinical teams can assess the resident and determine if a threat to their well-being is present, and act to prevent/reduce/manage it.

Behaviour Support in the Emergency Department: Supporting our Patients and Interdisciplinary Team
Project Lead: Melissa Laroche, Advanced Practice in Geriatrics
Organization: Queensway Carleton Hospital (Ontario)
Theme: Care Coordination & Navigation
Hospitalization is often stressful for patients in general, but when patients living with a cognitive impairment are faced with a new, unfamiliar environment, with unfamiliar individuals, it is common for behaviours to escalate and become unpredictable.
This innovative Behaviour Support Registered Nurse role in the Emergency Department will improve the care and mitigate the safety risks of our most vulnerable senior population who are living with dementia and are experiencing behavioural emergencies. Caring for complex patients such as individuals with neurocognitive disorders experiencing behavioural and psychological effects, does require specific knowledge, which is not always learned during our university education as clinical staff. We will be advancing practice by coaching the interdisciplinary team on how to care appropriately for patients in behavioural emergencies and empower them in their everyday practice through education that is adapted specifically to the ED setting.
Through the creation of the behaviour support RN role during his project we will be able to identify the specific patient safety risks relating to caring for patients with responsive behaviours in ED. This education will allow the interdisciplinary team in our ED to better understand triggers for behaviours, and appropriate interventions to mitigate, reduce, and manage these behaviours safely and effectively.
Increased and integrated knowledge and confidence for technology use with a focus on holistic health and wellbeing.
Project Lead: Cari McIlduff
Organization: University of Saskatchewan (Saskatchewan)
Theme: Aging in Place
Older adults recognize the need for increased technology use in their lives and health, but often lack confidence in their application. Previous CABHI funded work introduced new technologies to older adults of File Hills Qu’Appelle Tribal Council. Following this work, blood glucose monitors, blood pressure monitoring, smart scales, and tablets were introduced to older adults from Star Blanket Cree Nation (SBCN). Co-researchers of these projects, and the community’s Elders Council, have identified the need for further training in the use of technology and more accessible technology to monitor health and wellbeing.
This project seeks to integrate the learnings from previous and ongoing projects with SBCN to support older adults to continue to increase their confidence with technologies, specifically wearable technologies (Fitbits). Through the provision of technology that monitors activity levels, paired with fitness classes and tailored meal plans promoting Traditional foods, physical activity levels (and cognitive health) will be increased effectively and sustainably.
Smart Sheet: A soft flexible and stretchable tactile sensor array for the prevention of pressure injuries
Project Lead: Justin Wyss
Organization: University of British Columbia (British Columbia)
Theme: Aging in Place
The Smart Sheet is a soft, flexible, and stretchable tactile-sensor array sheet for pressure injury prevention, an injury risk for those sitting or lying in one place for too long, like individuals living with dementia. It can fit any shape and size, allowing it to cover areas of seats, wheelchairs, and beds. The device constantly checks the pressure on different body parts and collects this data. The data then appears as a heat map on smartphones or tablets, showing where the pressure is highest. The device has a special feature that uses this information to figure out which spots are most likely to develop injuries. It can alert users before any injury happens. This device helps prevent a severe, expensive health issue, making life better for those prone to these injuries, and reducing healthcare costs.
Taking charge of brain health: A webinar for older adults at risk of dementia
Project Lead: Keera Fishman
Organization: Baycrest (Ontario)
Theme: Aging in Place
Our goal is to provide older adults at risk of dementia with an immediate opportunity to engage in a self-directed and population-specific cognitive intervention. We aim to 1) provide evidence-based timely intervention to people who need it, 2) raise awareness about MCI and provide an introduction to the Learning the Ropes program, potentially driving access to the more fulsome program intervention, and 3)increase the accessibility of the Foundations session by creating an interactive webinar that can be accessed remotely at participants’ convenience. We will raise awareness/access to the webinar through Baycrest and our partners BrainXchange and Cogniciti. To promote international accessibility, we will translate the webinar into French and Spanish and ensure compliance with the Accessibility for Ontarians with Disabilities Act.
The EXALT cycle ergometer: A solution to maintain functional capacity in older adults
Project Lead: Eleonor Riesco
Organization: Université de Sherbrooke (Quebec)
Theme: Aging in Place
Staying during a prolonged period in a lying or seating position when hospitalized or during medical treatment (for example, during hemodialysis treatment) is associated with a high risk of functional decline and loss of independence in older adults, especially when frailty and dementia are present. To combat this, personalized exercise is key. But current equipment is often expensive or unsuitable.
The EXALT cycle is financially accessible, compact, and designed for safe use in clinical settings. It accurately measures exercise intensity and physical capacity. Plus, it comes with web portals for professionals/researchers to monitor and adjust workouts, and for patients/families/caregivers to view exercise data. The EXALT cycle makes in-bed exercise accessible, helping older adults maintain functional autonomy and enable them to maximize their independence.
Healthy Aging Brain Program: A Cognitive Decline Prevention & Awareness Program
Project Lead: Efan Gonsalves
Organization: Honsberger Physio+ (Ontario)
Theme: Cognitive & Mental Health
By identifying a gap in access to early screening opportunities for cognitive declines, paired with ever increasing clinical research studies regarding early onset brain changes, we have laid the foundations for ‘The Healthy Aging Brain Program’.
This program is designed to help with early identification of lifestyle and physical risk factors for cognitive declines such as dementia as well establish a current baseline of brain functional status. We have used our 35 years of clinical experience focusing on injury prevention & prediction, sport biomechanics, concussions and cognition paired with industry leading technology and diagnostic tools to create an accessible diagnostic identification and monitoring program to support practice innovation and advance the screening tools accessible to our communities. The focus of the program is to evaluate an individual’s current cognitive status as well as risk factors for possible cognitive decline.
Connect Rx: Solving social isolation through companionship and social prescribing while respecting the cultural and value of the seniors.
Project Lead: Dennis Natembeya
Organization: Louis Brier Home and Hospital (British Columbia)
Theme: Cognitive & Mental Health
Multicultural seniors yearn to voice their needs as they age in the community and residential homes. Currently, very little is being done to address the multicultural needs of seniors. Our platform will act as a gateway to provide cultural connection and a key component to implement socially prescribable activities to older adults. The platform will serve as a key partner in seniors’ health by improving their social engagement and mental stimulation through one-one activities implemented through the companion (link worker).
Our solution provides readily available companions that help seniors with social engagement and daily tasks in long-term facilities, all within a cultural context. Ultimately, through continued interaction with companions, older adults experience an improvement in their mood and depression.
Plum Tree “Virtual Live-At-Home” Assessments: Enabling People with Dementia to Live at Home
Project Lead: Linda Lee
Organization: Plum Tree Memory Care (Ontario)
Theme: Aging in Place
The Plum Tree virtual “Live-At-Home” Assessment tool is designed to help persons living with dementia age in place. The standardized workflow enables front-line primary care clinicians to identify and address potential risks and areas of need that can help to avert crises events and make daily life easier for people living with dementia and their carers. Specifically, the solution helps front-line primary care clinicians assess and make recommendations on aids to help with memory, household tasks, personal care, mobility, and eating and drinking difficulties in dementia care, as well as to assess problematic behaviours associated with advanced dementia that frequently lead to caregiver burnout.
A stress-relief robot
Project Lead: Lillian Hung
Organization: University of British Columbia (British Columbia)
Theme: Cognitive & Mental Health
Stress and anxiety are prevalent mental health conditions. Pre-pandemic data reported one in five Canadians experience a mental health disorder. During the pandemic, according to Statistics Canada (2022), from November 2021 to February 2022, 29.5% of older Canadians indicated that their mental health was worse than pre-pandemic.
This project proposes the development of a low-cost stress-relief robot that uses tactile senses to guide slow, deep breathing exercises to reduce stress. Features include smart sensors that can be installed to respond to users’ breathing in real-time, matching breathing patterns and gradually adjusting to the optimal rate for relaxation (8-10 breaths per minute with equal inflation and deflation).
The robot will wear a washable coating and can be dressed according to the user’s preferences. The robot will offer warmth and a soothing breathing rhythm to give a calming sensation. This low-cost, non-pharmacological, huggable robot will be accessible and useful to wide-ranging older adults to help manage stress and anxiety, improve quality of life, and promote health and well-being.

VR&R: Providing Respite to Caregivers by Managing BPSDs And Improving QoL in People with Dementia Using Immersive VR-Therapy
Project Lead: Lora Appel
Organization: OpenLab, UHN (Ontario)
Theme: Caregiver Support
“VR&R” is a Virtual Reality (VR) system that was initially conceived from feedback from over 200 individuals with dementia and their caregivers through multiple clinical trials across the spectrum-of-care (www.prescribingvr.com). VR&R immerses the viewer in different types of multi-sensory experiences: (1) 360-degree videos that simulate real-life environments (being by the ocean, watching a ballet), (2) simple and rewarding games, and (3) co-operative experiences where a loved one or volunteer can join in and interact remotely through a web-application. In order to have the system ready for prime-time, we will use this Spark grant to engage with end-users one more time to refine the usability and augment the system to ensure that it achieves our intended goals.
Expanding Memory Tools for Use in Culturally Diverse Populations
Project Lead: Komal Shaikh
Organization: Baycrest (Ontario)
Theme: Cognitive & Mental Health
Many Canadians experience memory difficulties, and the prevalence of memory disorders is rising both at home and around the world. To provide quality, patient-centered care to people experiencing memory changes, it is important to utilize measures that allow us to access patients’ own experience of memory change. Given that Canada has a large immigrant population, and many immigrants arriving here are older than 65 years of age, it is important that culturally appropriate memory tools are available to maximize detection of early cognitive changes and to minimize the burden of memory changes on daily life.
The objective of this project is to translate and adapt measures of memory change that were created by our group (i.e., the Multifactorial Memory Questionnaire and the Memory Impact Questionnaire) for use in culturally diverse populations. Comprehensive cognitive assessments are time intensive and expensive; therefore, it would be impractical to make such assessments available to all older adults who report memory complaints. Using self-report questionnaires to detect high risk candidates for further follow up is a low cost and quick way to ensure that cognitive assessments and interventions are made available to those older adults with greatest need. This information can be used on its own or combined with information about cognitive performance (e.g., performance on the MoCA) to further identify those who would benefit most from cognitive and lifestyle interventions.
Developing a Virtual Reality Companion for Persons with Dementia Living in Long-term Care
Project Lead: Andrew Frank
Organization: Bruyère Research Institute (Ontario)
Theme: Cognitive & Mental Health
Persons with dementia living in long-term care are at an elevated risk of social isolation, depression, and a lower quality of life. Our team has developed a computer-generated companion, presented using a virtual reality headset. The virtual companion engages the user in conversation by introducing herself and asking questions meant to stimulate reminiscence (e.g. “Tell me something about your childhood.”). Speech recognition software allows the virtual companion to listen and ask follow-up questions or add her own reminiscences, encouraging the person with dementia to converse further.